|
- Home
- BHTAC
The Behavioral Health Technical Advisory Committee (BHTAC) consists of seven members appointed by the following:
- KY Mental Health Coalition
- Kentucky Association of Regional Programs
- National Alliance on Mental Illness Kentucky
- A statewide mental health consumer organization
- People Advocating Recovery
- Kentucky Brain Injury Alliance
- Brain Injury Association of America – KY Chapter
The members of the TAC serve until their successors are appointed by the organizations they represent. Anyone interested in serving on this TAC should contact one of the organizations represented.
If you would like to receive information about the BHTAC meeting, please email kyadvocacy@gmail.com to make that request.
BEHAVIORAL HEALTH TAC REPORT TO THE MAC – JANUARY 25, 2024
-
The Behavioral Health TAC met via Zoom on January 11, 2024. All seven voting members were present, constituting a quorum. Also in attendance were Commissioner Lee and other representatives from DMS and Commissioner Marks and other representative from DBHDID. All six MCO’s were represented, as well as a number of members of the behavioral health community.
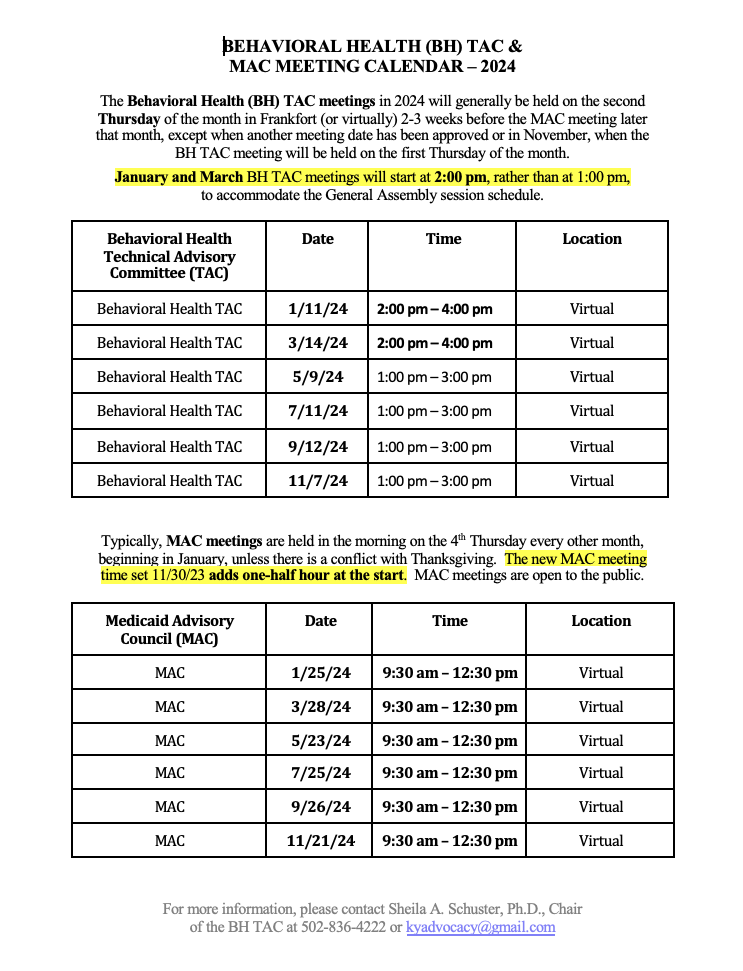
- The minutes of our November 15, 2023 Behavioral Health TAC meeting were approved which included our meeting dates for 2024.
- DMS Commissioner Lisa Lee shared a number of updates with the BH TAC, noting that 20 SPAs had been submitted to CMS in 2023 and all were approved! CMS had a recent site visit with DMS which was very positive and CMS requested that Deputy Commissioner Leslie Hoffman co-present with CMS staff at an upcoming Quality Conference on Behavioral Health. Kentucky is one of six states to be included in a collaborative focused on children and youth with high-acuity needs and she praised DMS’s collaboration with DCBS and DBH on initiatives such as this. Kentucky has also been applauded for its 12-month continuous eligibility for children.
-
SMI 1915(i) SPA (Waiver): Pam Smith reported that Town Hall meetings to explain the new SPA and to receive input were held in December at various locations across Kentucky. There were five meetings, with two of them also being offered remotely. DMS is in the process of reviewing the feedback, as well as updating their FAQ document. They are hoping to release the updated SPA application and begin the 30-day comment period on January 29th. Submission of the final version of the SPA to CMS will likely occur in March. Several attendees at the meeting had specific questions about the SPA which Pam and Leslie Hoffman responded to.
- Current 1915(c) Waiver Waiting List Numbers: There are currently 8,810 individuals on the Michelle P Waiver waiting list, none of them classified as emergency. There are currently 3393 individuals on the SCL Waiver waiting list, 86 of them classified as urgent (not emergency). These numbers reflect a modest increase in all categories: +26 in MPW; +37 in SCL, +5 Urgent. Pam also noted that the HCB Waiver is approaching having a waiting list, but does not yet have one. There is not currently a waiting list in either ABI waiver. There has been no change in access to therapy services, as they have not all moved to the State Plan yet. Some waiver participants are getting their therapy services under the SPA. In the acute ABI waiver. 264 of 383 slots were filled, with another 23 in the process of being enrolled. As a follow-up to an issue that Mary Hass had brought up at the last meeting about ABA services, Pam asked Mary to send information to her so she could look into the issue.
-
Reentry Waiver (formerly the SUD Incarceration Waiver): Angela Sparrow provided an update on this waiver which has completed the 30-day public comment period and the comments received have been responded to. No significant changes have been made to the waiver in the hope that DMS can get an earlier approval from CMS. Expansion to other populations and sites will be undertaken once the waiver is approved and implementation is underway. An Advisory Work Group has been appointed and will begin meeting soon to discuss implementation. Angela also noted that the 1115 SMI and 1115 SUD Waivers were submitted to DMS on Dec. 30, 2023.
- Rates: Victoria Smith with the Office of Data Analytics described the process that is being undertaken to evaluate every billing code listed in the BH Fee Schedule and to do a multi-state comparison for each code with regard to the rate and the way in which it is billed. This study is slated to be completed at the end of the month and the study will be shared with the BH TAC at our March meeting.
-
Regarding the plan by DMS to create a Behavior Health Associate (BHA) and to define their scope of practice, DMS has sent certified letters to each of the mental health licensure boards asking for their feedback on the proposal in terms of how it would impact (or not) their licensure laws and regulation. Since the deadline for receipt of these responses was to occur after our meeting, this agenda item was not discussed further and will be on our March agenda.
With regard to the dashboard to record “No Shows”, Justin Dearinger with DMS reported that he had requested a data report on what types of provider were posting data, but he had not received the requested information. He hopes to be able to share a report at our March meeting.
- Regarding the new mobile crisis services model, Leslie Hoffmann reported that a letter dated 1/3/24 was going out from DMS to all providers with information about implementation of the model. The Governor had announced the day before our meeting the awarding of seven grants to communities around the Commonwealth to establish Crisis Response Units (CRUs) in their locale. The goal is to limit the involvement of police or law enforcement in responding to behavioral health crises. She noted that 112 of Kentucky’s 120 counties are designated as “rural”, making crisis response more difficult. Kentucky is the first state to make these grants available. There will be another round of grants in the Fall and then annually thereafter.
- Sr. Deputy Commissioner Judy-Cecil presented a detailed PPT on the Medicaid Unwinding process, now underway for eight months, with the December data included. Flexibilities granted by CMS are being used to their fullest and while a number of Kentuckians have lost their Medicaid coverage, we still have 200,000 more covered than we did at the end of the PHE. CMS just recently asked every state to provide a 90-day look-back at pending cases which has required a good deal of staff time. New demographic data is now available by county. Enrollment in the Exchange insurance plans is up. The biggest issue is still the number of members who have not responded to the RFI and she asked everyone – family members, advocates, organizations and providers to reach out to members to remind them to respond!
- There was a follow-up discussion regarding Medicaid billing for behavioral health services provided to students. Justin Dearinger from DMS reported that there are on-going discussions between DMS, KDE and the Lt. Governor’s Office on the topic. There will be a survey going out later this month to school districts and providers both within the schools and in the community to try to get a better picture of how much is being billed, for what services and by whom. DMS is very interesting in increasing behavioral health services to students in schools and is eager to work with the districts to make it happen. We asked for a report of the survey results when they are available.
- Sheila Schuster gave a very brief update on the opening two weeks of the 2024 Regular Session of the Kentucky General Assembly. She noted several bills that have been filed which would potentially impact behavioral health – some positively, other negatively – is they were to pass. The Governor’s Budget has been released and filed as HB 114, but the House has not yet filed its budget, although it should be coming very soon.
- There are no new recommendations to the MAC at this time.
- New Business: DMS has issued an update to the MCO Provider Complaint form and this was posted and will be made available to BH TAC participants. There was also a question asked about whether a Workman’s Compensation claim could be filed for trauma-informed care for a worker who had experienced workplace trauma. Sr. Deputy Commissioner Veronica Judy Cecil volunteered to send some contact information.
- Old Business: The issue around an MCO’s continued questioning of the TCM reg and request for a recoupment from a provider is still unresolved. The latest correspondence will be shared by the provider with DMS so follow-up can be done.
- There were no issues raised about formulary or medication access concerns.
- The next meeting of the Behavioral Health TAC will be held on Thursday, March 14, 2024. The meeting will be held via Zoom from 2:00 – 4:00 p.m. Eastern Time so as not to conflict with legislative committee meetings.
- Thank you for the opportunity to provide this information to the MAC.
- Sheila A. Schuster, Ph.D.
Chair, BH TAC
BEHAVIORAL HEALTH TAC REPORT TO THE MAC – NOVEMBER 30, 2023
-
The Behavioral Health TAC met via Zoom on November 15, 2023. Five of seven voting members were present, constituting a quorum. Also in attendance were representatives from DMS and from DBHDID. All six MCO’s were represented, as well as a number of members of the behavioral health community.
- The minutes of our September 14, 2023 Behavioral Health TAC meeting were approved, as were the meeting dates for 2024.
-
SMI 1915(i) SPA (Waiver): Pam Smith reviewed the five meeting dates and cities where the SPA will be presented in-person to those present who will be able to ask questions and make comments. Two of the locations will also be accessible via MS Teams for those who are unable to attend in-person. A brief PPT was presented which gave information about the housing and related services options that will be available in the SPA for the individuals who meet the criteria. Ms. Smith pointed out that there will not be a cap on participants as is seen in the 1915(c) waivers, but only those individual who meet the requirement assessment criteria will be able to access the services. Exact locations for the meetings will be distributed in the near future.
Reentry Waiver (formerly the SUD Incarceration Waiver): Ann Hollen provided an update on this waiver which has now been opened for a 30-day public comment period. The stakeholder interviews have been completed and she noted that this waiver covers Behavioral Health (including mental health) and focuses on Social Determinants of Health for incarcerated individuals within 60 days of discharge into the community. Two remote information sessions are scheduled in late November and early Decembers to provide opportunities for interested persons who have questions about the waiver. The waiver will begin in the state’s 14 prisons and then will be extended to jails and to DJJ.
- Rates: This was a follow-up on a previous meeting’s agenda item. Comm. Lee distributed a copy of the SJR 54 (Part 1) report which will be made available to any interested person after the BH TAC meeting. Justin Dearinger described the rate-setting process as ongoing, with a list of changes and updates on rates being prepared for January 1st of each year. He said that they are constantly engaged with providers and others about changes in rates, with as many as 20 questions or requests coming in a single day. The process includes comparison reviews of other states’ Medicaid rates and commercial insurer rates, but the end result needs to stay within budgetary limits. In response to some questions, he reported that they utilize the appropriate TACs, individual providers and provider associations or groups for input on rates. Veronica Judy-Cecil noted that DMS meets with a SUD providers around rate issues periodically. She was then urged by the TAC Chair to meet with MH providers as well.
-
A new agenda item focused on DMS plans to create a Behavior Health Associate (BHA) and to define their scope of practice, which would include providing psychotherapy services to Medicaid members. BHAs would have a Bachelor’s degree in a human service field and would be working toward their advanced degree in a behavioral health field. They would work only in outpatient settings in CMHCs, BHSO, MSGs and CCHBCs and would only be able to work with this credential for five years. There were a number of questions asked about supervision, rates for their services and how they would be credentialed (apparently by DMS). There were also questions raised about the stance of the various MH licensure boards and DMS was urged to reach out to them to ascertain that. Questions were also raised about the appropriateness of Bachelor’s-educated individuals providing psychotherapy with such limited education.
With regard to the dashboard to record “No Shows”, Justin Dearinger with DMS reported that a letter had been sent to provider that very morning with information about accessing and using the dashboard, and encouraging all providers to record this important date.
- Pam Smith gave a short presentation on the 1915(c) waiting list numbers. There are currently 8784 individuals on the Michelle P Waiver waiting list, none of them classified as emergency. There are currently 3356 individuals on the SCL Waiver waiting list, 81 of them classified as urgent (not emergency). Of the individuals on the MPW list, 84% have Medicaid eligibility and 25% of those are receiving services on another waiver; another 4% are currently being enrolled in the MPW. Of the individuals on the SCL list, 93% have Medicaid eligibility and 65% of those are currently receiving services on another waiver; another 10% are in the process of getting enrolled in the SCL waiver. Mary Hass asked about the waiting list for the ABI waivers and was told that there was not currently a waiting list in either waiver. In the acute ABI waiver. 264 of 383 slots were filled, with another 23 in the process of being enrolled. In the long-term ABI waiver, 413 of 438 slots were filled, with 15 in the process of being enrolled. Mary brought up a problem area where the Behavioral Specialist who writes the treatment plan is prevented from doing the implementation and asked that this be looked into for resolution.
- Veronica Judy-Cecil reported that DMS was expecting the completion of a contract with an ASO to provide mobile crisis services across the state and was hoping for beginning implementation in the next month.
- Sr. Deputy Commissioner Judy-Cecil presented a detailed PPT on the Medicaid Unwinding process, now underway for six months. She emphasized a number of flexibilities that CMS had offered the states and that DMS was now taking advantage of. She also presented the timeline of the Appendix K flexibilities that were instituted for the 1915(c) waivers and will remain in place until those revised waivers have been approved by CMS and given a new effective date. In terms of Medicaid eligibility after going through the renewal process, 578,576 Kentuckians have gone through the renewal process, with 357,925 approved and 156,063 terminated. This yield an overall 60% approval rate. 57% of those who were terminated were for “procedural reasons” – they did not respond to the Request for Information. Reinstatements are available for a 90-day period after termination, so all are encouraged to reach out to those individuals and have them reply to the information request. Those who were terminated are being referred to kynect to obtain a Qualified Health Plan there.
- Sheila Schuster gave a very brief update on the 2023 Interim Session in terms of the Task Forces that have been meeting – notably, the CON Task Force, the School Safety Task Force and the CHFS Services Task Force. The Task Forces are wrapping up their meetings this month and we are awaiting the release of their findings and recommendations on December 4, 2023.
- There are no new recommendations to the MAC at this time.
- New Business: A question had been raised about possible barriers to school districts in billing Medicaid for behavioral health services provided to students. Justin Dearinger reported that DMS has had multiple discussions with various school districts through their Maternal & Child Health Branch to see why a fairly large number of districts are not billing Medicaid for these services. There has been information provided to districts and ongoing dialogue to make sure that there are no barriers to billing. Some of the larger districts are doing telehealth services. Joe Bargione, a school psychologist in attendance, noted that some districts use federal dollars to hire their behavioral health specialists and not able to bill Medicaid for their services. Veronica Judy-Cecil noted that DMS is very interesting in increasing behavioral health services to students in schools and is eager to work with the districts to make it happen. Dr. Bargione asked if there had been any increases noted by DMS in school billing for behavioral health services over the past few years? Justin Dearinger replied that he didn’t think there was an increase in the number of service providers, but there was an increase in the overall volume of billings. Some districts use CMHC and other community providers who do the billing. Bart Baldwin pointed out that KSBA has provided the Medicaid billing service for some schools. Karen Garrity noted that some schools would prefer to contract with the CMHC than to hire their own providers.
- Old Business: Follow-up was asked for from DMS on a question that had been raised at a previous meeting from a provider about an MCO’s continued questioning of the TCM reg and billing. DMS has indicated that they will follow up.
- There were no issues raised about formulary or medication access concerns.
- The next meeting of the Behavioral Health TAC will be held on Thursday, January 11, 2024. The meeting will be held via Zoom from 2:00 – 4:00 p.m. Eastern Time so as not to conflict with legislative committee meetings.
- Thank you for the opportunity to provide this information to the MAC.
- Sheila A. Schuster, Ph.D.
Chair, BH TAC
BEHAVIORAL HEALTH TAC REPORT TO THE MAC – SEPTEMBER 28, 2023
-
The Behavioral Health TAC met via Zoom on September 14, 2023. All seven voting members were present, constituting a quorum. Also in attendance were representatives from DMS and from DBHDID. All six MCO’s were represented, as well as a number of members of the behavioral health community.
- The minutes of our July 13, 2023 Behavioral Health TAC meeting were approved.
-
SMI 1915(i) SPA (Waiver): Leslie Hoffmann and Pam Smith from DMS stated that DMS staff will host a webinar on 9/25/23 to give information about the 1915(i) State Plan Amendment. When asked about the town hall meetings to be held across the state that had been announced at our July BH TAC meeting, Pam Smith stated that they will be sending out notices about the dates and locations and will give 30-days’ notice of those. When asked about a Public Comment period, she stated that in addition to the town hall meetings, there will be a 30-day public comment period on the SPA before it is submitted to CMS for their approval. Once again, BH TAC attendees expressed their great anticipation of seeing the services that will be provided for supported housing and supported employment for Kentuckians with SMI.
Reentry Waiver (formerly the SUD Incarceration Waiver): Angela Sparrow provided an update on this waiver which is being revised to meet new guidance from CMS. A question from an SUD provider about timeframes for reinstating an individual’s Medicaid coverage and restarting services is still outstanding. DMS is working with Myers & Stauffer on this waiver and they are currently conducting interviews with individuals and organizations dealing with reentry issues to gain insight into what is needed to make the transition from incarceration to community most supportive to the individual. Angela noted that this waiver covers Behavioral Health (including mental health) and focuses on Social Determinants of Health.
SMI 1115 Waiver Amendment: This waiver amendment has been submitted to CMS and we are awaiting any questions from them, following the close of the federal public comment period. This waiver has more hospital days for Kentuckians with SMI and a recuperative recovery program for a range of Medicaid members.
Request for Extension of the “Team Kentucky 1115 Waiver: This is still in CMS’s hands, with DMS waiting for further feedback from CMS. CMS has indicated that there will be a change in the date of the temporary extension to align it with the reentry waiver.
- Rates: The BH TAC had asked DMS a number of question about rates and Leslie Hoffmann brought some information to the TAC after she had discussed this with Commissioner Lee. She noted that there had been a recent rate increase to address issues with children in DCBS custody, focused on Psychiatric Residential Treatment Facilities (PRTFs). She also said that SJR 54 passed in the 2023 GA session required information from DSM about rates and rate-setting and had included behavioral health rates. That report is nearing completion and when it is finished, she will send it to the BH TAC so it can be reviewed and then discussed at our November TAC meeting. Ann Hollen answered a question regarding whether MCOs are required to pay the published rates and said that those rates are negotiated between the MCO and the provider and DMS does not play a role in that process, but they are required to pay at least the FFS rates. Angie Parker explained that if DMS told the MCOs the fee to pay, it would be considered a “Directed Payment” which has a lot of other requirements with it.
-
Justin Dearinger with DMS reported Good News that we have long awaited – the dashboard to report “No Shows” has been completed and is now available! However, because of security issues, it is not completely public, but open only to KY Health providers through a link on their DMS portal. He is hopeful that the security issues can be resolved at some point and that the dashboard will be more open to the public. [Will providers be notified that it is available?]
In another “Good News” development, Rosmond Dolen from KHA announced that the Single Point of Entry for Provider Credentialing went live at the end of August! It currently has participation from Aetna, Passport by Molina and Wellcare and they are hoping that others will also participate. A representative of United noted that they were trying to work through the complications of having multiple lines of insurance in the state before joining. Rosmond noted the importance of providers having their email addresses updated every 90 days to make sure that they were in communication with the CAQH Portal.
- Despite the work that DMS and DBHDID did to address the issue raised by one of the MCO’s of a different interpretation of the Targeted Case Management (TCM) regulation, 970KAR15:060 (which has been in place since 2015), there continue to be problems around this issue. At least one provider raised significant concerns at the meeting after they thought the issue has been resolved, and we have asked DMS to look further into the situation to make sure that the guidance issued by DMS is being followed by all of the MCOs and to assure that there have not been negative actions taken by any MCO toward a provider related to this issue. Steve Shannon, one of the voting members of the TAC, pointed out that TCM, which is a low-cost, but highly effective service for individuals with significant behavioral health issues, has been a source of discussion – and some disagreement – with the MCOs for years.
- Regarding changes in therapy services for individuals on the ABI Waivers, Pam Smith stated that the change to the state plan has not yet been approved by CMS, so there is no change in status at this time. Once approved, there will be a 90-day transition period. She does not believe that this issue will be resolved by CMS until November and will not actually take effect until after the first of the year. She affirmed that DMS will work with providers at that time to make a smooth transition to the State Plan. BH TAC Voting Member Mary Hass expressed concern that many of the most experienced and effective therapy providers have stopped providing services because of this change and the uncertain timeline for it. When the ABI Waiver is put out for public comment, Mary urged all interested in better services for individuals suffering a traumatic brain injury to advocate for the inclusion of cognitive therapy as a waiver service.
- Pam Smith informed the TAC that the Michelle P Waiver Comments will be delayed to include the Appendix K wind-down and DMS will provide training to consumers and family members on how to provide comments on the waivers. In response to a question about ABI therapy providers, Pam Smith indicated that she had not seen a change in utilization of the services. We had asked for an updated report on the waiting lists for the 1915(c) Waivers and Pam reported:
Michelle P – 8,639 with 48 placement slots available. DMS is working with DBHDID to review those on the waiting list and to move smaller groups into available slots one time a month. The SCL Waiver has a waiting list of 3,317, with none on the emergency list and 137 placement slots available for emergency placements. She stated that typically, 50% of those reached on the waiting list don’t follow through with a request for an assessment at that time. DMS is trying to more quickly turn over people waiting by having DBHDID take over the management of those two waiting lists. They are finding that many who signed up are unsure of what it is that they signed up for, some are getting services in other waivers, and 70-72% of the 8,600+ on the MPW waiting list are children under the age of 18 or 21. - Leslie Hoffmann reported that since the Mobile Crisis RFP is still in the bid process, there was not anything that she could report. She is hopeful that she can report more at the November TAC meeting and that the implementation of the program will not be much delayed beyond the original October 1 start date.
- Veronica Judy-Cecil gave a short PPT presentation on the status of the Medicaid Unwinding, from April 3, 2023 through the end of August, 2023. In July, of 54,975 renewals, 27,044 were approved and 20,344 were terminated with 7,587 pending. In August, of 54,344 renewals, 28,296 were approved and 18,662 were terminated with 7,386 pending. Since there is a 90-day reinstatement period available, she gave the number of individuals who were reinstated: May – 5,618; June – 4,758; July – 2,266 and the first 4 days of August, 433. She pointed out the Kentucky %ages of renewals and terminations look very similar to a number of other states. She urged providers especially to join with DMS and the MCOs to urge their patients to answer requests for information and to remind them of their renewal date. There was a flyer shown to the TAC members that can be downloaded in English and in Spanish to hang in offices, community centers and others places where Medicaid members might see it. She added that pharmacies are also joining in the effort to alert patients when they come in to reply to the renewal requests. DMS has sent letters and made at least 3 calls to each member about the process. CMS has a list of state strategies that they suggest and Kentucky has taken advantage of nearly every one of them.
- Sheila Schuster gave an update on the 2023 Interim Session in terms of both committee meetings and a number of Task Forces of interest to the behavioral health community. The CHFS Task Force has recently had testimony around the 1915(c) waivers; the CON Task Force will be hearing testimony on freestanding birthing centers; and the School Safety Task Force will soon hear testimony on mental health services in the schools and possible revisions of the district trauma-informed school plans to strengthen their focus on prevention and building resiliency. Each task force will submit its findings and recommendations to the Legislative Research Commission by December 4, 2023.
- Providers from several different perspectives reported that there have been no significant changes in the number of and requirements for MCO Audits – neither a notable increase, nor a notable decrease.
- There are no new recommendations to the MAC at this time.
- Old Business: There are some issues with payment for the new code, H0004, which was identified by DMS to cover the delivery of services in extended sessions. The report was that some MCOs were paying it and some were not. DMS will look into the issue. No new formulary issues were reports.
- The date of the next meeting of the Behavioral Health TAC has been changed from November 2nd to November 15, 2023. The meeting will be held from 1:00 – 3:00 p.m. Eastern Time via Zoom.
- Thank you for the opportunity to provide this information to the MAC.
- Sheila A. Schuster, Ph.D.
Chair, BH TAC
